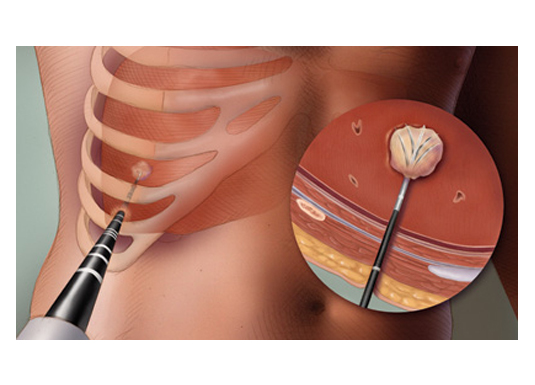
A swelling could develop anywhere in our body. It would be detected clinically by the doctor or by various imaging modalities like USG, CT or MRI. The swellings are commonly due to either infection or tumor (there are many other causes as well). The probable cause for the swelling may be guessed by imaging. However tissue sampling is must for confirmation, before starting the treatment. The swelling can be removed surgically and sent for examination to a pathologist and/or microbiologist. This however will require hospitalization, anaesthesia and also result in an ugly scar. The minimally invasive techniques for getting samples from these swellings are FNAC and Biopsy. These are predominantly done under local anaethesia and as outpatient procedures. Doing these procedures with image guidance (USG or CT) has two main advantages: one, tissue sample is taken from the swelling and not from the adjacent structures; two, we can avoid injuring the vital structures around the swelling. Thes
What is the difference between FNAC and biopsy?
In cases where infection is suspected the samples are sent to the microbiologist for identifying the organism and to identify the drug to which the organism is susceptible.
There are four potential outcomes for any guided sampling procedure:
Requirements for FNAC of superficial swellings:
Requirements for FNAC of deep swellings and for biopsy:
Additional tests may be needed as the case warrants.
Fluid can collect in many potential spaces in our body (pleural space in chest, peritoneal space in abdomen, abscesses any where in the body, post operative sites etc). These fluids have to be drained if infected or if they are causing mass effect over the adjacent vital structures. The fluid may also be removed to identify the cause. USG or CT can be used to guide to the needle placement into the fluid collection.
If the fluid is not expected to recollect, using image guidance a needle is placed into the collection and the fluid is aspirated. If the amount of fluid is more or if it is expected to recollect a tube (catheter) is left in place, so that the fluid can be let out as when it collects. By leaving the catheter in place repeated aspirations can be avoided.



Few painful inflammatory conditions of joints and tendons are relieved by injection of a mixture of steroid and local anesthetic agents. Traditionally this is done blindly in which we are not sure where the medications are getting deposited. Now with image guidance the deposition of the medications can be seen live as we inject.




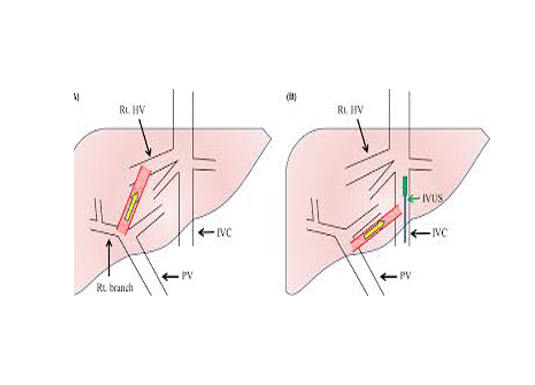
Few patients who need a liver or a renal biopsy have a greater tendency for bleeding complications. In such patients the biopsy is performed from the endovascular side, so that, if at all bleeding happens it is into the blood vessel itself and not out side.
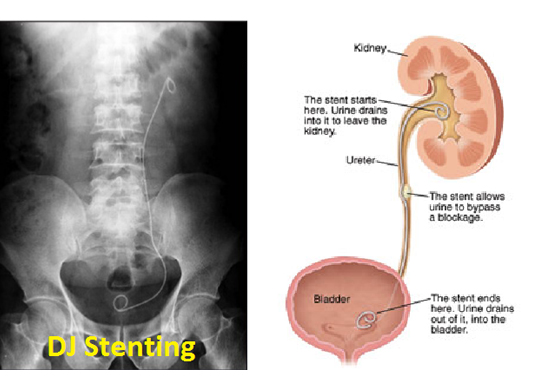
Blood is filtered in the kidneys and urine is formed. The urine formed in the kidneys passes to the urinary bladder through the ureters. When there is a block in the path along the ureter, urine stagnates. This urine stagnation has two adverse effects – it damages kidneys and stagnant urine predisposes to infection. The block has to be relieved as early as possible. This is done by the urologists from below under general anaesthesia. In patients where this is not successful or the general condition of the patient is not suitable for general anaesthesia the block can be bypassed from above by an interventional radiologist. This process called “percutaneous nephrostomy” can be done under local anaesthesia. A tube called catheter is placed through which the urine comes out of the body into a collecting bag placed outside the body. A stent can also be placed in the ureter so that urine formed proximal to the block bypasses the block and enters the urinary bladder, this process is called ‘antegrade ureteric stenting’. Similar blocks in the outflow of the urinary bladder can be relieved by percutaneous cystostomy till the permanent treatment is done.



Liver secretes bile which aids in digestion. Bile is collected from liver and temporarily stored in gall bladder after which it is delivered into the small intestine. A block in its path results in jaundice and predisposes to life threatening infection. A block closer to the small intestine is treated by endoscopy. If this procedure fails or if the block is away from the small intestine, the block can be treated from the skin side. This procedure is done by an interventional radiologist. A plastic catheter is placed in the dilated biliary tract. The other end of the tube is outside in which bile is drained out of the body. If feasible a plastic tube or a metal stent is placed across the block opening it. Thereby the bile is not wasted and instead drains into the intestine like anybody else.

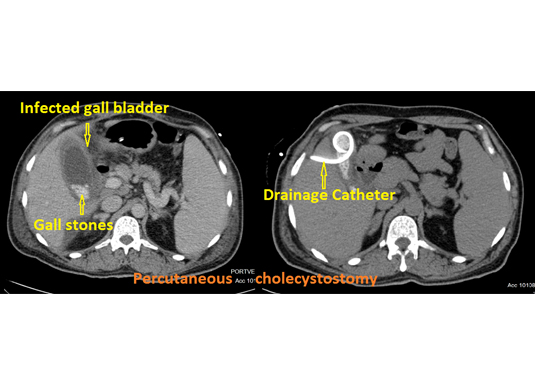
Acute cholecystitis is a condition where the outlet of the gall bladder is blocked by a stone and the gall bladder is infected. The treatment of choice is removal of the gall bladder (cholecystectomy) which is done under general anaesthesia. Patients whose general condition is not favorable for surgery can be treated by a procedure called percutaneous transhepatic cholecystostomy. In this procedure the contents of the gall bladder are drained outside by placing a catheter.

Varicose veins:
There are two sets of veins in our legs, a deep one and a superficial one, both function together to return blood from legs to heart against gravity. The two major superficial veins namely great saphenous vein and lesser saphenous vein open into the common femoral and popliteal veins respectively. The unidirectional valves at their junctions may not function well and result in blood returning to the legs via the superficial vein. This results in the appearance of prominent veins in our legs which are termed varicose veins. The long term consequence of varicose veins is leg edema, discoloration, itching and ulcer formation. There are many other causes for varicose veins and a Doppler study is done to identify the treatable causes. If the deep system is normal and the varicose veins are due to valve incompetence the entire vein can be ablated so that the causative patho-physiology is removed. With time all the above mentioned changes disappear.

DVT:
Blood flows slowly in the veins. In predisposed individuals the blood may clot (Deep vein thrombosis - DVT) in the deep veins of leg (popliteal and femoral), pelvic deep veins (iliac veins) and the abdominal deep vein (Inferior vena cava). The treatment of choice is administration of an anticoagulant. In acute setting this clot can potentially dislodge and move into the lung vessels resulting in a condition called pulmonary embolism, which is an emergency. If there are free floating clots in these large veins and the general condition of the patient is such that he or she cannot withstand pulmonary embolism, a mechanical filter can be placed in the inferior venacava which will hold on to the dislodged clot. These filters are removable and are removed later on when the risk becomes low.
IVC filter placement & IVC filter retrieval
One of the long term complications of DVT is called post thrombotic syndrome where the venous return from the leg to the heart is severely hampered. It is characterized by leg edema, discoloration, itching and ulcer (Post thrombotic syndrome - PTS). These blocked veins can be opened up using venoplasty and stenting techniques. Venoplasty is a procedure in which a high pressure balloon is inflated inside a narrowed vein to increase its diameter. When the diameter achieved is suboptimal and in certain other conditions a stent is placed to keep the vein open.
In order to protect a patient from PTS the DVT may be treated in the acute setting with clot dissolving medicines (urokinase, rTPA etc). However there is a downside for this treatment as the same medicine may induce a bleeding anywhere else in the body. These clot dissolving medicines when administered locally into the clot the risk of bleeding is lower. This is done by an interventional radiologist who inserts a multi side hole catheter into the clot and administers the medicine continuously over a period of time. Mechanical clot busting may also be done to speed up the clearing of clot.


Dialysis access interventions:
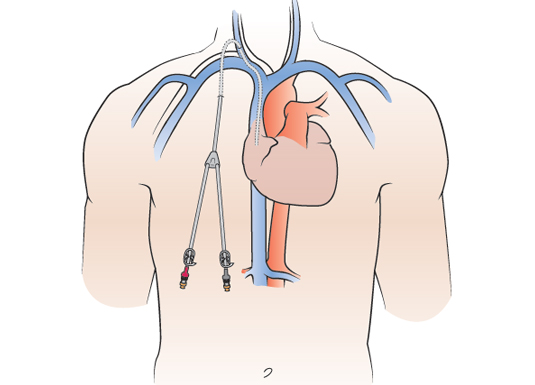
Patients who have renal failure need dialysis - a process by which the kidney function is done by a machine outside the body. For this blood has to be removed out and after filtering it has to be sent back into the body. Commonly this is done by creation of a fistula between an artery to a superficial vein in the arm. It takes approximately 6 weeks to be ready for dialysis use. Till then a double lumen catheter is placed in the neck. This can be used immediately after placement. The catheter could be non tunneled or tunneled. The non tunneled catheters are seen protruding out in the neck and are often associated with complications like infection and block. The tunneled catheters are known to be better with lesser short and long term complications. These tunneled catheters are inserted by Interventional Radiologists. Shown below are few cases of tunneled catheters.



A fistula is meant for use till kidney transplant is done. It may take years before a patient can undergo kidney transplantation. Fistula malfunction is a known entity where there may be blocks in the fistula. Similarly in patients whom direct neck catheters were introduced in the past may develop block in the central veins that transfer blood from the arms to the heart. Both these conditions are associated with inadequate dialysis, inability to access the fistula and prolonged bleeding. These blocks can be opened up using a balloon by a procedure called as venoplasty which is performed by interventional radiologist. In severe cases the opened up segment of vein may close immediately. In such cases an extra support is provided to the wall by placing a stent.




Central venous accesses:
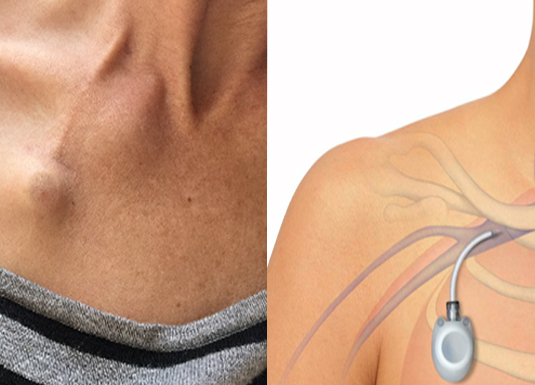
Many of the tumors and some of the infections need long term administration of intra venous medicines. A peripheral line (commonly called as venous cannula) can be used for short term only, after which it gets displaced, blocked or infected and cannot be used further. A new cannula is secured each and every time these medicines are administered. Soon all the peripheral venous accesses are lost and further injections will not be possible. If long term venous access is anticipated placement of Chemoport and Hickman catheter is advisable to avoid a situation where all the peripheral veins will get exhausted. These also provide greater degree of comfort. Here a tube is placed with one end close to the heart. The other end exits through a long subcutaneous tunnel in the chest. This long tunnel offers stability and also protects from infection. Through the external end blood can be withdrawn for analysis and medicines can be administered. The external end of the tube could be buried beneath the skin as in Chemoport or could be hanging in the front of the chest. A peripherally inserted central venous catheter (PICC line) is a combination of both, wherein the line runs up a vein in the arm and ends in a large vein in the chest.












RFA













The nervous system has a complex blood supply. There are many diseases that could affect the blood supply resulting in functional and life loss. Neurointerventions involve the treatment of these diseases.
Just as coronary angiography helps us identify the diseases of the blood supply to the heart, digital subtraction cerebral angiography (cerebral DSA) helps us to assess the blood supply to the brain. It is done under local anaesthesia and in a cathlab. It involves placement of a plastic tube called catheter through the groin into the arteries of the brain. Dye is injected through the catheter and images are obtained.
Paralysis is a condition that results when blood supply to the brain is blocked. There is a very short time window during which the block has to be opened. If it is not opened within that time frame, the paralysis becomes permanent. The procedure where the clot is removed is called Mechanical Thrombectomy.
Few of the patients with mild paralytic symptoms recover and this is called as transient ischemic attack (TIA). A partial block in the blood supply has to be ruled out by various imaging modalities. And if there is a significant block the lumen can be restored by dilating the segment with balloon and placing a stent.


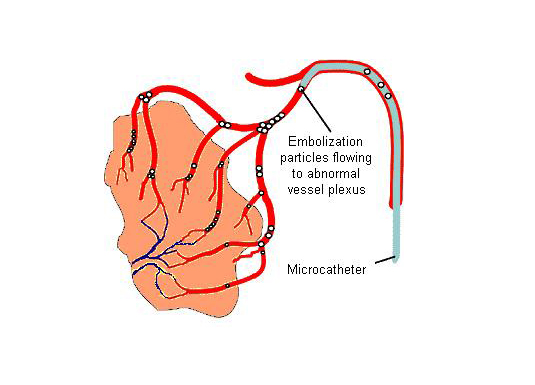
The above procedures are called revascularization procedures in which the diseases reduce the blood flow to brain and we improve the flow to brain. There are few conditions where there is increased blood flow and we attempt reduce the flow. This procedure is called embolization. The conditions are Arterio-venous fistula and arterio-venous malformations.
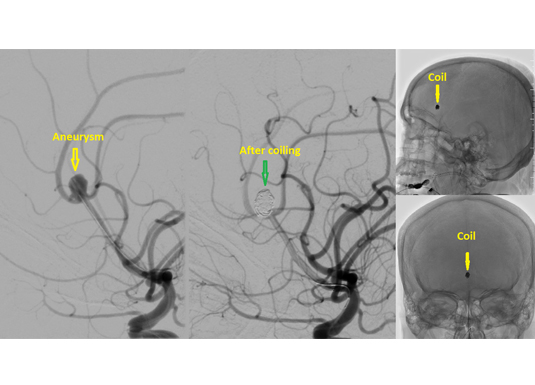
The arteries to brain may become like a balloon and burst inside the head. Such patient experiences the worst headache of their life. The balloon is called as an aneurysm. This condition is potentially fatal and has to be treated by embolization. We enter the aneurysm from the inside and fill it with coils. Blood does not enter the aneurysm after coiling and thereby eliminates the risk of the aneurysm bursting.
Cerebral venous stenting
The blood is taken to the brain from heart by the arteries. Then blood is returned to the heart by the veins. If there is a block in the draining veins pressure builds up in the head and this could result in headaches and visual disturbances. There are drugs which reduce the pressure and this helps to a certain extent. For those patients who do not improve with medicines the block can be opened up with a stent.

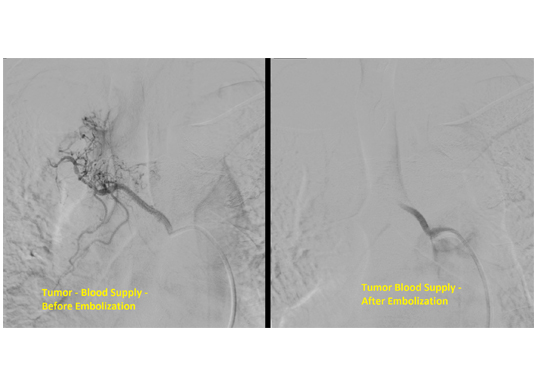
Spinal angiogram is done to assess the blood supply to the spinal cord. Below is a case of tumor with increased blood supply from a spinal artery. As the surgical removal is associated with increased blood loss, the blood supply was blocked of endovascularly.

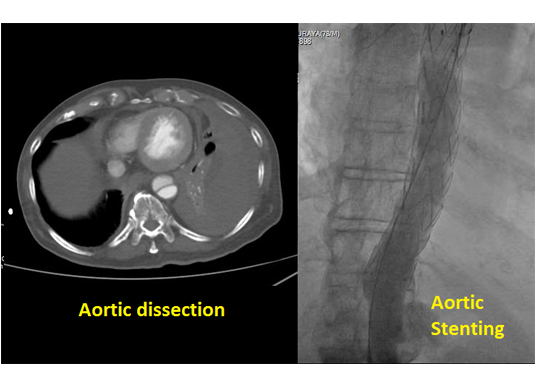
Aortic: Graft stenting of aortic aneurysm / dissection
Aorta is the large main artery that carries blood from the heart to all the parts of the body. Aortic aneurysm is a condition where its lumen is over dilated with increased tendency for a fatal rupture. We place a covered stent (almost resembles a flexible hose pipe) through this dilated segment thereby giving it additional support and normal size. In few patients even if aorta is of normal caliber its wall could be diseased and may perforate (aortic dissection). This hole can also be closed by reinforcing its wall with a covered stent.
Percutaneous
Vertebroplasty
As we age the bones become fragile and break, particularly the vertebral bodies. In the initial days of fracture the fracture fragments rub against each other and cause severe disabling pain. The pain can be relieved by injecting bone cement along the fracture lines thereby stabilizing the fragments. This procedure is called vertebroplasty.

Biliary disorders:
Bile is formed by the liver and is passed on to the intestines where it helps in digestion. Bile also carries along toxic substances that need to be removed from the body. If its passage is obstructed due to any cause it accumulates in the body and results in jaundice. MRI is prescribed to locate the level and cause of obstruction. In patients for whom a curative surgery is not possible stents are placed to open up the block. Sometimes bile is let out through a tube extending from the biliary system to the skin. This procedure is called percutaneous transhepatic biliary drainage.

Few of the patients who have stones in their gall bladder get infected. Surgical removal of the gall bladder is the treatment of choice. Their general condition may deem them unfit for surgery and in these patients a procedure called percutaneous cholecystostomy. Here the infected bile in the gall bladder which is under pressure is drained outside by a plastic tube. Once the general condition of the patient improves this tube is removed and the definitive surgery is performed.
Blood is filtered in the kidneys to form urine. Urine then moves along a passage called the collecting system which includes ureters and urinary bladder. When this pathway is obstructed due to any reason urine is retained within the system and pressures builds up. This raise in pressure hinders normal functioning of kidneys and it fails. The retained urine could get infected. The treatment involves removing the obstruction when possible. In cases where removal of the cause is not immediately possible the urine can be temporarily diverted out of the body by placing a tube through the skin. This procedure is called percutaneous nephrostomy. If possible a stent can be placed across the obstruction with one end above and the other end below the obstruction. This procedure is called DJ stenting. Both these procedures are done under local anaesthesia and are life saving many a times. Similarly a tube can be placed in the urinary bladder through the skin when its outflow is obstructed and this procedure is called percutaneous cystostomy.